Day 1 :
Keynote Forum
Adrian Baranchuk MD FACC FRCPC
Queen`s University, Canada
Keynote: Case Reports contribute to knowledge translation
Time : 09:00-09:30

Biography:
Dr. Adrian Baranchuk, a native of Buenos Aires, Argentina, obtained his MD from the University of Buenos Aires in 1990. After qualifying in Internal Medicine and Cardiology at Sanatorio Mitre, Buenos Aires (1995), he completed a Clinical Fellowship in Cardiac Electrophysiology at the same institution under the supervision of Dr. Claudio Muratore.
He completed his Clinical Fellowship (1997) and joined the Arrhythmia Service until 2002 when he immigrated to Spain to join the Arrhythmia Service at the Fundacion Jimenez Diaz; working as a Research Fellow in the Animal Lab under the supervision of Dr. Jeronimo Farre. For his work in this lab, he was awarded with the 3rd Chinchona Award (Sponsored by 3M Foundation). During his stay in Madrid, Spain, he received a grant (as PI) from MAPFRE MEDICINA Foundation (Madrid, Spain). (Ultrasonic Analysis of Radiofrequency Lesion of the Pulmonary Venous Wall through Three-dimensional Intravascular Echography: Therapeutical Implications for Atrial Fibrillation Ablation).
Dr. Baranchuk was appointed as a Clinical Fellow in Electrophysiology at McMasterUniversity in September 2003, under the supervision of Drs. Carlos Morillo and Stuart Connolly. In 2004, he won the 1st Prize at the Fellows Forum, “5th Annual EP Fellows Course” (Sponsored by Medtronic) held in Montebello.
Dr. Baranchuk was appointed as an Assistant Professor of Medicine at Queen’s University to join the Division of Cardiology in June 2006. He is an active member of the Arrhythmia Service and has founded the EP Training Program in 2007. Currently the program has 3 Clinical Fellows.
In 2009 he received his cross-appointment with the Department of Physiology and Biomolecular Sciences.
His scholarly activity work includes sleep apnea and cardiovascular disease, specifically the link between sleep apnea and cardiac arrhythmias, complex ablation, cardiac devices and Electrophysiology and Electrocardiology education. He is a member of numerous editorial boards and reviewer of several journals. The recipient of a teaching award (Outstanding Contribution in the Core Internal Medicine Program) and nominated in 2009, 2010 & 2012 for teaching awards from the Faculty of Health Sciences. He is a member of the Mentorship Program at Queen’s University.
Dr. Baranchuk has been very active presenting his work at national and international meetings. In the last 4 years, he visited Argentina, Chile, Colombia, Venezuela, Russia, Brazil, Poland, Germany, Spain, USA; and several places in Canada.
His first book, Atlas of Advanced ECG Interpretation, has been recently released (REMEDICA, UK) and represents a big collaboration effort from well-recognized electrophysiologists of all around the world.
He has published more than 200 articles in well-recognized international journals, 20 book chapters and presented more than 150 abstracts all around the world.
He was promoted to the rank of Associate Professor of Medicine and Physiology in 2010.
Abstract:
Will be updated shortly
Keynote Forum
Jennifer L. Doherty-Restrepo, PhD, LAT, ATC
Florida International University, USA
Keynote: Does simulation-based training increase athletic training students’ clinical confidence and competence of performing a cardiovascular screening?
Time : 10:00-10:30

Biography:
Jennifer Doherty-Restrepo is a Clinical Associate Professor and Chair of the Department of Athletic Training in the Nicole Wertheim College of Nursing and Health Sciences at Florida International University. Her areas of expertise include andragogy, simulation-based instruction, and professional as well as continuing education in athletic training. Jennifer serves the Athletic Training Profession as a manuscript reviewer for the Journal of Athletic Training and the Athletic Training Education Journal. She is an Associate Editor for the Athletic Training Education Journal. Jennifer serves the Commission on Accreditation of Athletic Training Education as a site visitor. Additionally, she is the Chair of the University and College Athletic Training Student Committee of the Athletic Trainers’ Association of Florida. In recognition of her service and contributions to athletic training education, Jennifer was the recipient of the 2015 Athletic Trainers’ Association of Florida University and College Athletic Trainer of the Year award.
Abstract:
Context: The need for increased screening to detect cardiac diseases in preparticipation physical examinations is a focus in athletic training. Objective: To examine if a simulation-based training can increase athletic training students’ self-reported confidence and clinical competence in conducting a cardiovascular screening. Design: Pretest-posttest design. Participants: 25 first-year athletic training students. Intervention(s): Standardized cardiovascular curriculum. Main Outcome Measure(s): Learner self-reported confidence scale, multiple-choice knowledge exam, and objective structured clinical examination (OSCE) of cardiovascular assessment skills and auditory recognition of heart murmurs. Results: Self-reported confidence increased significantly from 4.4±2.1 to 9.2±3.0 post-intervention (F = 78.7, p < 0.001) with a moderately high effect size (h2=0.789). Knowledge exam scores increased significantly from 11.0±2.5 to 13.6±4.0 post-intervention (F= 5.3, p= 0.031) with a low effect size (h2=0.191). The history-taking assessment of the OSCE increased significantly from 2.6±1.6 to 5.7±1.7 post-intervention (F= 70.1, p< 0.001) with a moderately high effect size (h2=0.751). The clinical skills assessment of the OSCE increased significantly from 4.1±2.8 to 15.6±1.6 post-intervention (F= 415.4, p< 0.001) with a high effect size (h2=0.952). Conclusions: Simulation-based training is an effective tool for increasing students’ self-reported confidence and competence in conducting a cardiovascular screening.
Keynote Forum
Denis Larrivee
Loyola University Chicago, USA
Keynote: Contemplative revelations: Higher faculties in global nervous system integration
Time : 10:30-11:00

Biography:
Dr. Denis Larrivee is a Visiting Scholar at Loyola University Chicago and has held professorships at the Weill Cornell University Medical College in New York City and Purdue University, West Lafayette, Indiana. A former fellow at Yale University's Medical School and Department of Biology he received the Association for Research in Vision and Opthalmology's first place award for studies on photoreceptor degenerative and developmental mechanisms. He is the current editor of a text entitled Brain Computer Interfacing and Brain Dynamics with InTech Publishing and an editorial board member of the journals Annals of Neurology and Neurological Sciences (USA) and EC Neurology (UK). An International Neuroethics Society Expert he is the author of more than 50 papers and book chapters in such varied journals/venues as Neurology and Neurological Sciences (USA), EC Neurology (UK), Journal of Neuroscience, Journal of Religion and Mental Health, and IEEE Explore.
Abstract:
Contemplative meditation reveals a latent capacity for personal integration that enhances mental and physical heath through relational and transcendent ordering. Studies of a related meditative practice, mindfulness, reveal, for example, not only positive phenomenological benefits but also substantive physical changes in underlying neural and bodily factors, which are correlated with the duration and frequency of meditative practice. The extended intentional focus of contemplative meditation acquired from the Christian legacy, and then evolved in its later development, implicates an even greater breadth of neural deployment that assists personal integration. They suggest, thereby, a scope of disciplinary consolidation that exceeds that of mindfulness and so likely activates a broader and corresponding range of integrative processes that are latent for implementation as needed. The role played by the brain and nervous system in the self integration of higher faculties, however, is neglected in current philosophy of science models that guide empirical neuroscientific praxis; these latter, rather, are premised on the brain's mediation of coherent and coordinative operation instead of the systemically mediated, mutually constraining influences of peripheral and central neural networks. Indeed, results from contemplative meditation suggest that body and brain are unified through their ordering to higher systemic and ontological ends. Bodily performance in and through intentional actions, for example, shapes the brain and body's neural architecture to yield an integral performance unit. In like manner, higher faculties, like personal identity and intention, emerge from the extended peripheral network throughout the body to unify the whole individual in actions, such as those promoted in contemplative meditation. This paper will pursue an evidence based presentation, discussing the underlying neural events through which self autonomous actions promote and assist personal integration.
Keynote Forum
Russell D Weisz
Delray Medical Center, USA
Keynote: Extracellular matrix xenografts in the treatment of open fractures of the extremities with large soft tissue defects
Time : 11:00-11:30

Biography:
Russell D Weisz is a board certified orthopedic surgeon who began his medical training at the State University of New York Health Sciences Center at Brooklyn where he graduated Magna Cum Laude. He then completed his orthopedic surgical residency at the Hospital for Joint Diseases/New York University and concluded his training with a one-year fellowship in orthopedic traumatology at Tampa General Hospital. Dr Weisz is the director of orthopedic trauma at Delray Medical Center, a level one trauma center in Palm Beach County Florida. He specializes in the treatment of complex fractures and the reconstruction of fractures that have not healed or have become infected. Dr Weisz is a clinical affiliate Assistant Professor at the Department of Surgery, Florida Atlantic University, Charles E Schmidt College of Medicine. Dr Weisz is involved in clinical research and is a principal investigator of the study “Assessing the efficacy of IV ibuprofen for treatment of pain in orthopedic trauma patients”.
Abstract:
Introduction: Application of biologic scaffolds such as extracellular matrix (ECM) products is a promising trend in the treatment of complex wounds in orthopedic trauma patients without the use of flap coverage.
Patients and Methods: Study included a cohort of patients with open fractures of bones and large skin defects. Wounds were complex in nature based on one of the following: 1) vascular injury with tissue ischemia, 2) large skin and soft tissue defects in challenging areas (e.g. plantar weight bearing aspect of the heel, high mobility zone of the antecubital fossa, etc.), 3) large area of exposed bone with no viable local rotational flap coverage, 4) type IIIB open tibia fractures. All patients underwent sequential debridements with provisional external and definitive internal stabilization of the skeletal injuries. Sequential xenograft applications of porcine urinary bladder ECM products (Cytel Wound Matrix and MatriStem MicroMatrix, ACell Inc. Columbia, MD) were performed from 2 to 4 times in each patient. In all patient’s negative pressure wound therapy (NPWT) was utilized.
Results: In all patient’s stable soft tissue coverage was achieved after xenograft implantation and regeneration of the granulation tissues which was followed by the split-thickness skin graft (STSG). Multiple applications of the ECM provided soft tissue coverage to a degree which alleviated the need for flap placement. In one area (heel) complete closure was achieved with the use of ECM sheets alone and without subsequent STSG.
Conclusions: The clinical outcomes demonstrated that even in challenging cases where local flap coverage of bone or neurovascular structures is not possible, sequential xenograft implantation allowed to achieve a stable soft tissue envelope. Different forms of ECM products are easy to apply in the presence of orthopedic hardware. In certain wounds, the complete closure can be achieved even without subsequent skin grafting. We recommend the relatively early application of xenograft.
Keynote Forum
Franz Muller
Hospital Barmherzige Bruder, Germany
Keynote: Peri-implant femoral fractures: The risk is more than three times higher within the proximal femoral nail compared with dynamic hip screw
Time : 09:30-10:00

Biography:
Franz Müller is Consultant and Senior Surgeon in the largest catholic hospital in Germany. He is specialist in all kinds of orthopedic trauma incl. spine and pelvic, as well as endoprosthesis incl. revision surgery. He is first and senior author of more than 20 original papers, especially in spine surgery and trauma. In his vacations he is also working for Medecins Sans Frontieres.
Abstract:
Introduction: Information is lacking regarding incidence rates, treatment regimens, and outcomes concerning peri-implant femoral fractures (PIF). Therefore, we performed a retrospective study to provide scientific data concerning the incidence and outcome of PIF following osteosynthesis of proximal femoral fractures (PFF).
Material & Methods: We retrospectively included all patients who received osteosynthesis for PFF between 2006 and 2015 and in whom PIF was confirmed postoperatively. All available patients with PIF were contacted minimum one-year post-surgery.
Results: A total of 1.314 osteosynthesis procedures were performed, of which 705 were proximal femoral nails (PFNs), 597 were dynamic hip screws (DHSs), and 12 screwed appliances only. During the same period, 18 PIFs (1.4%) were reported. However, PIF was 3.7 times higher within PFN when compared to DHS (15/705:2.1% versus 3/597:0.5%; odds ratio: 3.7). The following analysis also included 8 patients with PIF who were referred from other hospitals, resulting in a total of 26 patients. Mean patient age was 84.8 years (range, 57–95), with a predominance in female (23x) and in the left femur (19x). PIF occurred after an average of 23.6 months (range, 1–81) post-surgery. The fractures, most of which were spiral-shaped, were most commonly treated with locking plate osteosynthesis. The surgical revision rate was 7.7%, and the one-year mortality was 23.1%. At an average of 43.0 months (range, 12–100) post-surgery, it was possible to contact 18/26 patients (69.2%), and their mean Parker Mobility Score was 5.2 points (range 2–9).
Conclusions: Peri-implant femoral fracture is a rare incident within the old age traumatology of PFF. However, based on our small number of cases, it occurred within PFN much more frequently compared with DHS. Locking plate osteosynthesis has been shown to be effective and reliable. Surgical revision and mortality rates do not appear to be increased when compared to those with the initial treatment of proximal femoral fractures.
- Sessions: Anaesthesiology | Autopsy | Cancer Science | Cardiology | Clinical Pathology | Dentistry | Dermatology and Skin Care | Diabetes | Critical Care and Emergency Medicine | Epidemiology | Forensic and Legal Medicine | Gastroenterology | Geriatric Medicine | Internal Medicine | Microbiology | Neurology | Obstetrics and Gynaecology | Ophthalmology | Orthopaedics & Rheumatology | Paediatrics | Pathology- Anatomy & Clinical | Pharmacology and Therapeutics | Psychology | Public Health | Pulmonology | Radiology | Sexual Health | Surgery | Toxicology | Urology | Vascular and Endovascular Surgery | Veterinary | Women’s Health | Miscellaneous Case Reports
Location: Hall-01
Session Introduction
Ronish Gupta
McMaster University, Canada
Title: Rapid resolution of high-output chylothorax with reduction of spinal subluxation

Biography:
Dr. Ronish Gupta is a pediatric intensivist at the McMaster Children’s Hospital and an Assistant Professor with McMaster University. He completed medical training at Queen’s University in Kingston, Canada. This was followed by residency and fellowship training at the University of Ottawa, Canada. His academic interests revolve around medical education, and include critical care simulation, interprofessional curriculum development, and resident selection. He also regularly utilizes noteworthy case reports as a means of scholarship and teaching.
Abstract:
Case Description:
A 2-year-old generally healthy boy with a history of limping gait presented and was admitted to a community hospital with severe Influenza A illness. There, he was intubated for refractory hypoxia, and found to have large bilateral pleural effusions. Bilateral chest tubes were inserted, draining > 1 L of milky fluid combined. He was transferred to the regional pediatric intensive care unit. With the effusions drained, he was easily extubated and biochemical testing confirmed the fluid to be chyle (triglyceride level = 3.48 mmol/L). Computed tomography scanning of the chest and abdomen was subsequently negative for malignancy, but incidentally found rib fractures, scapular fracture, and an unstable spinal subluxation (T11-L1). In the interim and during spinal surgical planning, the high-output chylothorax continued despite several days of NPO status with total parenteral nutrition (> 1L/d or > 50mL/kg/d). Following reduction and partial fixation of the spinal subluxation, the pleural drainage immediately ceased. Within 24-hours following surgery, the drainage became < 50mL/d. Two weeks later, the chylous drainage remained absent with the patient on a full enteral medium-chain triglyceride containing diet.
Discussion:
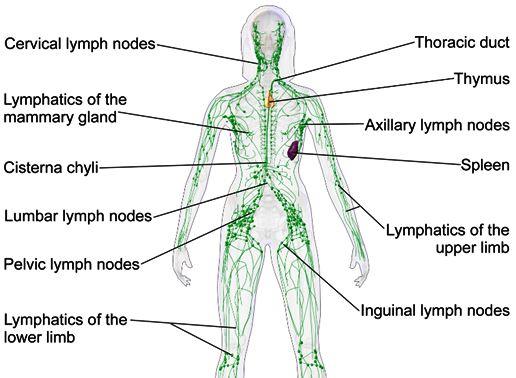
Acquired chylothorax in pediatrics is typically associated with mediastinal pathology (e.g. trauma, infiltrative), obstruction of drainage, or abnormal lymphatic vessel development. Case reports of chylothorax developing following spinal trauma and manipulation exist. This is, however, the first report to our knowledge of chylothorax resolution as a result of spinal intervention. Potential mechanisms include relief of obstruction of the cysterna chylii, the large lymphatic reservoir typically located adjacent to the L1-L2 vertebral bodies. Patients with chylothorax in the context of thoracolumbar spinal pathology may warrant consideration of an intervention aimed at relieving any potential lymphatic obstruction.
Recent Publications
1. Pillay TG, Singh B. A review of traumatic chylothorax. Injury. 2016;47(3):545-550. doi:10.1016/j.injury.2015.12.015.
2. Bender B, Murthy V, Chamberlain RS. The changing management of chylothorax in the modern era. Eur J Cardio-thoracic Surg. 2016;49(1):18-24. doi:10.1093/ejcts/ezv041.
3. Ichikawa Y, Sato A, Sato K, et al. Chylothorax associated with child abuse. Pediatr Int. 2015;57(6):1202-1204. doi:10.1111/ped.12707.
4. Mora de Sambricio A, Garrido Stratenwerth E. Chylothorax following anterior thoraco-lumbar spine exposure. A case report and review of literature. Rev Española Cirugía Ortopédica y Traumatol (English Ed. 2015;59(2):129-133. doi:10.1016/j.recote.2015.01.002.
5. Gartside R, Hebert JC. Chylothorax following fracture of the thoracolumbar spine. Injury. 1988;19(5):363-364.
Amir S Lotfi
Tufts University School of Medicine, USA
Title: The distal left radial artery access for coronary angiography and intervention: A new era

Biography:
Amir Lotfi is an associate professor of medicine, Tufts University School of medicine in the cardiology division at Baystate Medical Center. His training in coronary, carotid and peripheral interventions. His area of interest includes radial intervention, coronary physiology, coronary imaging, and ischemic preconditioning.
Abstract:
Statement of the Problem:
Patients' intra and post procedural comfort, quick recovery, as well as procedure success, are key elements for choosing the right arterial access site. Radial artery access has been of increasing interest since it was first described. Advanced treatments of coronary lesions, from primary percutaneous interventions during ST elevation myocardial infarction cases to chronic total occlusion cases, have been increasingly done through the radial access. Distal left trans radial artery (dlTRA) is a new technique first described by Kiemineij. We report the first documented US experience of the left distal radial artery access for coronary angiography and interventions.
Methodology & Theoretical Orientation:
dlTRA was attempted on 22 consecutive patients, consented for a cardiac catheterization. 7 patients underwent percutaneous coronary intervention. The left hand is prepped in the usual fashion, exposing the anatomical snuff box. Under ultrasound guidance, the artery is punctured and the sheath is inserted carefully. The cardiac catheterization is completed using standard diagnostic and guiding catheters that are typically chosen for femoral artery access. Haemostasis was achieved with a radial band. Patients had the ability to use the right hand as well as bend their left wrist post procedure.
Conclusion & Significance:
dlTRA was successful in all 22 patients. 7 patients underwent PCI through this approach. Two patients required a multi vessel complex PCI with multiple stents and additional equipment. There were no conversions to the right radial or femoral approach. All patients had excellent haemostasis with a radial band, with no complications. Pre discharge radial pulses were intact in the wrist as well as in the anatomical snuff box. Distal left trans radial access is feasible and safe in patients that are carefully selected and are deemed good candidates. There is a learning curve for developing such program, as is the case with conventional radial access.
Cristina Rossi
San Giacomo Hospital, Italy
Title: Postnatal outcomes following Prenatal Diagnosis of Placental Mosaicism: Case Reports from Literature
Biography:
A Cristina Rossi has received her Medical Degree in 1998 and Residency in Obs/Gyn in 2003. She is an author and reviewer of peer-reviewed journals. Her interest is in prenatal diagnosis and twin pregnancy. She is a Consultant in Obs/Gyn at Ospedale della Murgia (Bari, Italy).
Abstract:
Mosaicism is a rare genetic condition that occurs when two or more populations of cells are chromosomally different. The association between mosaicism and phenotypic abnormalities varies widely according to the degree of mosaicism and the genetic anomaly. Mosaic cells can affect fetal tissue, might be confined to the placenta or may involve both the fetus and placenta. Prenatal detection of mosaicism is obtained by amniocentesis or chronic villous sampling (CVS) and represents a clinical dilemma, since only case reports or very small series are described in literature. In addition, articles reporting about mosaicism focus on the genetic disease rather than the effects of mosaicism. We therefore performed a review of literature in order to pool case reports and small series and obtain a large sample size, which is essential for studying and counselling parents about a rare condition, such as mosaicism.
For this purpose, we selected articles that were based on prenatal detection of mosaicism by invasive procedures and obtained placental and fetal karyotype postnatally or postmortem. From each case of mosaicism described in literature the following outcomes were abstracted: location of mosaicism (fetal and/or placental), type of mosaicism (numerical or structural), invasive prenatal procedure, survival rates and perinatal outcomes. Survival rates were defined as newborns alive and well within 28 days from birth. Perinatal outcomes were defined as presence of fetal malformation, intrauterine demise, termination of pregnancy, and postnatal examination or autopsy, and were stratified according to the characteristics of the mosaicism.
From 33 articles, 36 cases of mosaicism were pooled. Of these, 20 (55.5%) were confined to fetal tissue, 11 (30.5%) to the placenta and 5 (14.0%) were both fetal and placental mosaicism. Fetal mosaicism was observed with amniocentesis (18 cases; 90.0%), CVS (1 case; 5.0%) or umbilical cord sampling (1 case; 5.0%) and was either structural (5 cases; 25.0%) or numerical (15 cases; 75.0%). All but one fetus presented major malformations. Six fetuses (30.0%) had single malformations and 14 fetuses (70.0%) presented multiple anomalies. Fourteen pregnancies (70.0%) were terminated, 1 pregnancy (5.0%) ended with fetal demise, and 1 neonatal death (5.0%) occurred because of prematurity, leaving 4 infants (20%) alive and well.
Placental mosaicism was observed with amniocentesis (8 cases; 72.7%), or CVS (3 cases; 27.3%) and was either structural (1 case; 9.0%) or numerical (10 cases; 91.0%). Three fetuses (27.2%) were growth restricted. There were 1 fetus (9.0%) with transposition of great vessels and 3 (27.2%) fetuses with minor malformations. Two pregnancies (18.2%) were terminated, 1 (9.0%) neonatal death occurred for prematurity, and 8 (72.8%) liveborns were normal.
In the 5 cases of both fetal and placental mosaicism, prenatal diagnosis was obtained by amniocentesis (3 cases; 60.0%) and CVS (2 cases; 40.0%). Four pregnancies (80.0%) were terminated because of major malformations and 1 fetus (20.0%) was apparently normal but developmental delay appeared in infancy.
This review shows that the majority of mosicism forms affects fetal tissue, which, in turns, is associated with a high risk of fetal malformations. Furthermore, in 70% of cases fetal defects were so severe that termination of pregnancy was performed. In addition, we observed that 20% of neonates were born alive and well and only one infant presented mild defects. Mosaicism confined to the placenta appears to be associated with a better prognosis. According to our review, the partial involvement of the placenta might result in fetal growth restriction in about one third of cases, probably because the genetic anomaly cannot ensure a regular intrauterine growth. Only one fetus presented a major congenital heart disease, whereas most of the babies (72%) with placental mosaicism were normal and the unique neonatal death was related to prematurity rather than placental insufficiency.
The finding that fetal mosaicism is more severe than placental mosaicism is further confirmed by the fact that when both the two conditions are present, 80% of pregnancies are terminated due to severe malformations.
Fetal karyotype by umbilical blood cord sampling or fetal biopsy should be performed to differentiate placental from fetal mosaicism, although this approach might not be efficacious in all cases, because the mosaic cell lines might not involve fetal hematopietic cells. In addition, umbilical cord sampling and fetal biopsy might be complicated with infection, miscarriage and premature rupture of membranes. Parents should be counselled that when prenatal diagnosis of mosaicism is made, a definitive diagnosis to exclude or ascertain fetal involvement is not actually feasible.
Nataliia Grygorieva
F Chebotarev Institute of Gerontology NAMS of Ukraine, Ukraine
Title: Bone mineral density (BMD), Fracture Risk Assessment (FRAX) and Trabecular bone score (TBS) indices in postmenopausal women with different types of osteoporotic fractures

Biography:
N Grigorieva received Medical Degree in 1994 and PhD degree in 1999 at Odessa Medical University (Ukraine). Since 2000, she worked in the Department of Clinical Physiology and Pathology of Musculoskeletal System at DF Chebotarev Institute of Gerontology NAMS Ukraine. She completed primary training in rheumatology and is now a rheumatologist of the highest qualification. Since 2017, she is Full Professor of medicine. Her researches focused on experimental modeling of bone and joint diseases, bone and joint pathology and women aging, premature aging, and rehabilitation. She is a Secretary of the Ukrainian Scientific and Medical Society of Gerontology and Geriatrics and a President of "Ukraine without osteoporosis and fractures" Patients Association. She is a member of Editorial Board of Ukrainian and foreign journals, author and co-author of over 350 publications in national and international journals, more than 10 monographs, more than 30 national guidelines, newsletters, and patents.
Abstract:
Introduction: Bone mineral density (BMD) and Trabecular bone score (TBS) are independent parameters of bone which effectively predict osteoporotic fractures risk. FRAX® and adjusted FRAX by TBS are simple calculators which assess 10-years probability of major osteoporotic (MOFs) and hip fractures (HF). Their significance was confirmed in various studies, however, information depending on the type of osteoporotic fractures is limited.
Purpose: The purpose was to study indices of FRAX®, BMD, TBS and adjusted FRAX by TBS in postmenopausal women with different osteoporotic fractures. We examined 275 women aged >50 years, which were divided into two groups depending on previous fractures presence. The patients of the 2d group were divided according to fracture localization: Vertebral fractures (VF), Humerus fractures (HF), Ulna/radius fractures (URF), Wrist fractures (WF). BMD and TBS were measured by X-ray absorptiometry (Lunar, Prodigy), assessment of risk factors was performed by FRAX® and adjusted FRAX by TBS. FRAX scores with body mass index (BMI), BMD and TBS were calculated.
Findings: It was established that BMD of the lumbar spine/total body and TBS indices were significantly lower only in patients with VF compared to women without previous fractures (WPF) in contrast to patients with other fractures. BMD of femoral neck/total hip did not differ in any group with fractures compared to control. In addition, indices of FRAX/BMI-MOF were significantly higher for women independently of the type of fractures, however, FRAX/BMI-HF were reliably higher only at women with VF and URF compared to parameters of women WPF. FRAX/BMD-MOF and FRAX/TBS-MOF indices were significantly higher at women independently from the type of fractures except for women with HF. Parameters of FRAX/BMD-HF and FRAX/TBS-HF were higher only in patients with VF.
Conclusion & Significance: FRAX® and adjusted FRAX by TBS are important indices for fractures risk assessment in postmenopausal women with previous fractures which propose additional information without BMD measurement.
Isa Abdi Rad
Urmia University of Medical Sciences, Iran
Title: Spectrum of MYO15A mutations and report of a Novel Splicing Mutation in an Iranian Family with Sensorineural Hearing Loss

Biography:
Isa Abdi Rad was born in Iran in 1962. He received his M.D. degree from Tehran University of Medical Sciences in 1991 and his Ph.D. degree in Medical Genetics and also Fellowship in Neurogenetics from University of Nottingham, England in 2002. In 2003, he joined the department of Medical Genetics, Urmia University of Medical Sciences, as an Assistant Professor then became Associate Professor in 2008 and Professor in 2013. Prof. Isa Abdi Rad is member of British Clinical Genetics Society, American Society of Human Genetics, and Iranian Neurogenetics Society. Currently he is a Professor of Neurogenetics and head of Medical Genetics Department of Motahari Teaching Hospital, Urmia University of Medical Sciences, Iran. His primary research interests are in the field of neurogenetics and dysmorphic disorders.
Abstract:
Autosomal recessive non-syndromic hearing loss is a genetically heterogeneous defect which affects millions of people in the world. In this study‚ we performed clinical exome sequencing in a patient with a non-syndromic sensorineural hearing loss and found a novel mutation (c.9611_9612+8del) in MYO15A gene which creates a shift in the reading frame starting at codon 3204. The new reading frame ends in a stop codon 16 positions downstream. This variant has been confirmed by Sanger sequencing and the family analysis showed the mutation segregates with hearing loss.
To the best of our knowledge, this mutation has not been reported in any data base.
Introduction
Non-syndromic sensorineural hearing loss (SNHL) is the most common sensorineural disorder accounts for ~70% of hereditary hearing loss which 80% of cases have an autosomal recessive mode of inheritance (ARNSHL)[1].To date, Over 60 genes and more than 100 genetic loci have been identified for ARNSHL (Hereditary Hearing Loss Homepage, http:// hereditaryhearingloss.org). The genes GJB2, SLC26A4, MYO15A, OTOF, and CDH23 are most commonly implicated in ARNSHL[2].
MYO15A Mutations (NM_016239) have been reported to cause sensorineural hearing loss in human [autosomal recessive 3 (DFNB3)][3]. The DFNB3 locus (OMIM-600316) was first identified in an isolated village in Indonesia where 2% of their population had affected by hearing loss Then, another study identified a causative role for MYO15A gene mutation in DFNB3[4].MYO15A have 66 exons spanning 71 kb of DNA on chromosome 17p11.2[5].
The MYO15A mRNA transcript encodes a 3530 amino acid protein (myosin XVa), which has MyTh4 (Myosin-Tail like Homology region 4) domains, FERM (4.1 protein, Ezrin, Radixin, and Moesin) motifs, a SH3 (Src Homology 3) domain, and the PDZ domain. Myosin-XVa is a critical protein for tip localization of whirlin and differential elongation of hair-cell stereocilia and organization of actin within the hair cells of cochlea so Myosin-XVa is an important element in normal auditory function[6].
There are several linkage analysis studies about mutations of MYO15A causing ARNSHL in consanguineous families from specific countries, such as Pakistan, Turkey, and Iran[7-9]. Mutations of MYO15A at the DFNB3 locus are the second cause of autosomal recessive non-syndromic deafness in Iranian population[7, 9]. In the present study, we reported a novel MYO15A mutation identified by clinical exome sequencing in a consanguineous Iranian family with ARNSHL. To the best of our knowledge, this mutation has not been reported in any database.
Materials and methods
A 22 years old female with hearing loss was referred to Medical Genetic Department, Urmia Medical University, for detection of any possible hereditary hearing loss mutation. Parents were consanguineous with F=1/16 (first cousin) and clinical examination exclude dysmorphic features. Audiometric records were compatible with sensorineural hearing loss, so non-syndromic sensorineural hearing loss was confirmed.
Molecular analysis was performed after obtaining informed consent. Sanger sequencing for the common deafness genes, that is, GJB2 and GJB6, was negative. Clinical exome sequencing was performed on a single proband case. After preliminary detection of mutation by Clinical exome sequencing, PCR amplification and Sanger sequencing were performed to verify that the identified mutation co-segregate with the phenotype in the studied family. In addition, detected mutation was searched in healthy controls database for the same ethnic group (Iranome; http://www.iranome.ir/).
Evolutionary conservation of the sequences and structures of the proteins and nucleic acids was assessed Using the 1000 Genomes Project database, and the ExAC (Exome Aggregation Consortium) browser.
Results
A novel homozygous mutation c.9611_9612+8del (p.Leu3204Cysfs*17) found at exon 58 of MYO15A in a consanguineous Iranian family with a case of non-syndromic sensorineural hearing loss. (fig1) This mutation creates a shift in the reading frame starting at codon 3204. The new reading frame ends in a stop codon 16 positions downstream. The deletion is in close proximity to the highly conserved donor splice site of exon 58. This mutation has been confirmed by Sanger sequencing. It is classified as likely pathogenic (class2) according to the recommendations of ACMG. Using the 1000 Genomes Project database and the ExAC (Exome Aggregation Consortium) browser, candidate pathogenic variants were defined as splice-site and frameshift mutation.
The mutation was determined to be heterozygous in her parents. The c.9611_9612+8del was not found in healthy controls database for the same ethnic group (Iranome; http://www.iranome.ir/). This novel mutation is predicted to disrupt the function of the myosin XVa protein, which is integral to the mechanosensory and neurosensory activity of hair cells in the inner ear.
The alignment of MYO15A from different species of human, chimpanzee, monkey and cattle was analyzed. The result proved that this region was conservative among multiple species which highly suggesting that these residues are important for the proper protein function.

Biography:
4
Abstract:
5
Mahyar T. Nouei
Ferdowsi University of Mashhad, Iran
Title: Functional Loss and Gain in Older Adults: Insights from Data Analytics

Biography:
Mahyar Taghizadeh Nouei, was born on December 8, 1973 in Shemiran, Tehran, Iran. He is a Ph.D of Applied Mathematics-optimal control and optimization at Ferdowsi University of Mashhad, Iran. He received his MSc in Engineering of Information Technology from Tarbiat Modares University and his BSc of Mathematics Applied in Computer in Shahid-Beheshti University, Tehran, Iran.
He has involved in several national and regional projects as a System Analyst and Team Leader( ie Core Banking Solutions), and He has taught more than 130 courses for students in Payam-e-Noor University of Tehran province faculty of computer.
Abstract:
Very little information is available to guide patients, providers, families and policy makers regarding expectations for the sequence of, likelihood and time to functional loss and recovery of the activities of daily living (ADLs). Moreover, without benchmarks to gauge the time to improvement or decline in the functional abilities, it is difficult to assess the effectiveness of the intervention for recovery of functional loss. Using a combination of various machine learning algorithms and 1.8 million observations which were collected from 300,000 residents of the US Veteran Administrations Community Living Centers, we provide a data-driven analytical model of functional status change for residents in nursing homes. Particularly, we analyze the likelihood, number of days until, and sequence of functional decline, recovery, and death after each ADL. Our cross-validated predictions are very accurate in majority of cases. We have made all the results available to public through our web calculator www.disabilityforecast.com. Establishing such a patient-centric benchmark is vital to ensuring optimal care for persons in nursing home settings. This information here can help in planning for end-of-life disabilities.
Harinarayan C V
Sakra Hospitals, India
Title: Ectopic parathyroid adenoma - Single centre experience from India

Biography:
Prof. Dr. C.V. Harinarayan is an excellent clinician, accomplished research scientist, astute bed-side investigator, exemplary organizer and administrator. He has made pioneering contribution and played a key role in placing the specialty of endocrinology on the global map. His work is distinguished service of a high order. He has many indexed publications in reputed journals and his work is cited by many researchers (1065 cites/year). His research work is quoted in many textbooks of metabolic bone disease has provided new perspectives in the correct diagnosis and treatment of metabolic bone diseases. His documentation on the low vitamin D status as the cause of bone disease in primary hyperparathyroidism, documentation of the low vitamin D levels in urban and rural subjects through population survey, his work on dietary calcium and vitamin D status of Indian population potentially changed the Recommended Dietary Allowances (RDA) of India has paved the way for fortification of Food with vitamin D in the country especially for those who are indoors for most of the day. His work of the renal tubular damage as the cause of bone disease in fluorosis is ranked top 10 publications - year 2006 by Internet. He has indigenously developed intact IRMA radioimmunoassay for parathyroid hormone in India along with BARC Mumbai and was a co-chair for development of “Clinical Practice Guidelines on management of Postmenopausal osteoporosis (2012-13) – Executive summary and Recommendations” for Indian Menopause society. His in vitro studies on ampoule model of previtamin D synthesis has shown that we as Indians can synthesize enough vitamin D on exposure to sunlight from 11 am to 2 pm, by exposing 10 to 15% of body surface area for 15 to 30 minutes. He also showed that correction of vitamin D deficiency can improve the pancreatic beta cell secretory function.
Abstract:
Introduction:
The Commonest cause of primary hyperparathyroidism (PHPT) is hyper-functional parathyroid adenoma (PA)(94%) hyperplasia(<6%) rarely parathyroid carcinoma(<1%). Parathyroidectomy is a definitive cure with a success rate of 95 %. Less than 15% have one or more hyper-functioning glands in the ectopic location.
Materials and Methods:
Between 2014 to 2017, seven of the 13 patients with PHPT and failed non-invasive localization were included for the study. Hybrid localization techniques with PET/CT and newer tracer agents (11C-methionine) were used. Locations of parathyroid adenoma were classified using Perrier classification which uses letters A-G to describe the exact location of the adenoma. A 50 % drop in PTH levels as compared with pre-incision values was confirmed as cure.
Results:
The biochemical and hormonal profile of the 7 patients with ectopic PA are (mean+SD) serum calcium (mg/dl), 25OH-D (ng/dl) and PTH (pg/ml) 11.36+0.82;22.82+8.57; 205+105 respectively. Forty three percent (3/7) had renal stones. In all seven patients PA was localized using PET/CT scans and tracer agents 11C-choline. The profile of PA were two type-G (intra-thyroidal), one type-C (posterior mediastinum), two type-F (Superior mediastinum), one of type D(mid region of posterior surface of thyroid parenchyma at the junction of recurrent laryngeal nerve and the middle thyroidal vein).
Conclusion:
Ectopic PA is rare. In a biochemically and hormonally confirmed PHPT and failed imaging localization techniques/failed neck exploration one should look for ectopic PA. Newer hybrid techniques combined with newer tracer agents (PET scan) will help in localization of PA. To the best of our knowledge this is the first report of series of ectopic PA from a single centre from India.
Biography:
Veral Vishnoi graduated with a Bachelor of Medicine, Bachelor of Surgery with Honours from James Cook University in Queensland, Australia. He is currently working part-time as a surgical registrar at the John Hunter Hospital in Newcastle whilst completing his PhD with the University of Newcastle in New South Wales, Australia. His research interests lies in colorectal surgery in particular diverticular disease.
Abstract:
We present an 80-year-old gentlemen (with a virgin abdomen) who was admitted with acute chylous ascites in the context of a closed loop small bowel obstruction. Acute chylous ascites is characterized by extravasation of lymphatic fluid into the abdominal cavity. Just over 100 cases have been reported in the literature since 1910. Cases are described as either obstructive, traumatic or idiopathic. Acute chylous ascites often presents as an acute abdomen with the majority of the reported cases progressing to either a laparotomy or laparoscopy, during which copious amounts of chlye was encountered on entering the abdomen, a precipitating cause was not always apparent. Our patient clinically had a small bowel obstruction with radiological evidence of thickened loops of small bowel in the abdomen and free fluid. The patient required a laparotomy as conservative management failed. On entering the peritoneum copious amounts of chlye was unexpectedly encountered. The patient had a congenital band adhesion causing a closed loop jejunal obstruction, there was no other pathology identified. In the absence of any obvious lymphatic obstruction we hypothesized that the venous congestion associated with a closed loop small bowel obstruction caused increased lymphatic pressures leading to extravasation of chlye into the abdomen. This case highlights the diagnostic uncertainty associated with an acute chylous abdomen as well short and long-term management goals.
Ilina Micheva
Medical University of Varna, Bulgaria
Title: Aggressive blastic plasmacytoid dendritic cell leukemia with central nervous system involvement : a case report
Biography:
Ilina Micheva is a medical doctor, specialist in Internal diseases and Clinical hematology. She is an associate professor in the Medical university of Varna and a head of the Transplant Unit in the Hematology clinic, University hospital, Varna. Her PhD study is based on the role of dendritic cells in the pathogenesis of myelodysplastic syndromes. She has published several papers in reputed journals in the field of hematology, immunology, gene therapy.
Abstract:
Blastic plasmacytoid dendritic cell leukemia (BPDCL) is a rare, clinically aggressive hematologic malignancy derived from the precursors of plasmacytoid dendritic cells and characterized by co-expression of CD4 and CD56 without other lineage-specific markers. Its misleading clinical presentation resembles many other aggressive diseases like myeloid, lymphoid, NK neoplasms and malignant melanoma.
Our patient was a 67-years-old male who presented with complains of asthenia and diffuse generalized rash of blackish palpable plagues on his back, chest and hands that have appeared 5-6 months before hospitalization. He had no B symptoms, no lymph adenomegaly and hepatosplenomegaly. The CBC showed leukocytosis (22,93.109/L), anemia (Hb-75 g/L) and thrombocytopenia (36.109/L). The blood smear and bone marrow revealed 45 % and respectively 70 % of blasts with morphological characteristics of lymphoblasts. Flow cytometry showed a CD45low population expressing CD4, CD56, CD303, CD304, and high levels of CD123 and TCL1. There was no T-cell, B-cell or myeloid expression except for CD33 and CD2. Karyotype was normal. CT revealed mediastinal and abdominal lymphadenomegaly and splenomegaly.Treatment according to Hyper-CVAD protocol was initiated. A week later the patient became somnolent and bradypsychic. MRT revealed multiple bilateral hyperdense lesions with perifocal edema. In two days the patient passed out.
BPDCN could be hardly distinguished from several hematological and oncological neoplasms. Despite its low incidence, clinicians should include it in differential diagnosis of tumors with cutaneous, blood, lymphatic tissue and CNS involvement. The early diagnosis with intensive chemotherapy and CNS prophylaxis may improve the outcome.
Zehara Hamdihun Essa
Bahir Dar health science college, Ethiopia
Title: Pygopagus parasiticus twin; pathogenesis of human true tail revealed; an extremely rare case report
Biography:
Zehara Hamdihun has completed medical education at Bahir Dar University at the age of 23 years and started postgraduate study on obstetrics and gynecology in this year. I am interested on maternal health and I have started researches on maternal health last year, I hope it will contribute some to maternal health in the future.
Abstract:
Background: - Conjoined twins are one of the rare developmental anomalies, where twins do not separate completely. They are of two types, symmetrical the common type and asymmetrical the rarest. Asymmetrical twins are of two types, one is parasitic twin (heteropagus) and the other is fetus in fetus. The incidence of heteropagus (parasitic) twin’s is less than 1 per 1 million births.We report Pygopagus parasiticus twin of unique presentation. Case presentation: - Parasitic conjoined twin born from 28 years old primigravida lady through spontaneous vaginal delivery at gestational age of 35 weeks and 4 days after she was admitted with the diagnosis of preterm premature rupture of membrane to Felege Hiwot referral hospital in Bahir Dar, Ethiopia. Upon examination, the parasite twin (enlarged embryo) of 58mm CRL and 30gm weight attached to the viable autosite through 110 mm long and 6 mm diameter tail like structure extending from caudal part of the embryo (parasite) to the skin overlying the sacral area 10mm left lateral from the midline. The parasite (enlarged embryo) has embryonic structures at about 5 weeks. Ultrasound and x-ray was done to the autosite and there was no associated gross congenital anomaly. After parents’ request for cultural and cosmetic reasons, the parasitic twin was separated by minor surgical excision. The autosite discharged well and it was in good health at postpartum visits. Conclusion: - An extremely rare co-incidence of parasitic twining as human true tail is reported and it may give evidence in the controversial pathogenesis of conjoined twin. It also helps us to widen our views on pathogenesis of human true tails. Some of case reports on human tail can be ruminants of the twin process that has arrested at early embryonic age or lost its distal component by ischemic resorption rather than the true human tail.
